5 Things to Know Before Starting Suboxone Treatment
This entry was posted in Addiction Recovery and tagged 5 things to know about suboxone treatment, what you need to know about suboxone treatment on June 23, 2020 by Justin Baksh, MS, LMHC, MCAP, Chief Clinical Officer.


Imagine yourself clean and sober, surrounded by clean and sober friends. Imagine living in a safe, welcoming environment with a job that pays the bills. Imagine enjoying restored family relationships and a life that gets better and better. If you are struggling with opioid addiction, Suboxone treatment can help get you there.
Qualified addiction programs that offer counseling and support along with Suboxone treatment can transform every aspect of your life. If you are considering Suboxone treatment, here are five things you need to know:
1. Suboxone treatment relieves withdrawal symptoms and cravings
As one of the most addictive substances in the world, opioids are notoriously difficult to stop taking.
In fact, it only takes five days of continuous opioid use to experience withdrawal when you stop. Debilitating symptoms can start within just six hours of your last dose.
From depression and anxiety to insomnia and seizures – being “dope sick” is no picnic. As one former user shared:
“For many users, full-blown withdrawal is often foreshadowed by a yawn, or perhaps a runny nose, a sore back, sensitive skin or a restless leg. For me, the telltale sign that heroin was wearing off was a slight tingling sensation when I urinated.
These telltale signals — minor annoyances in and of themselves — set off a desperate panic: I’d better get heroin or some sort of opioid into my body as soon as possible, or else I would experience a sickness so terrible I would do almost anything to prevent it: cold sweats, nausea, diarrhea and body aches, all mixed with depression and anxiety that make it impossible to do anything except dwell on how sick you are.
You crave opioids, not because you necessarily want the high, but because they’d bring instant relief.” (Rinker, 2019)
Fear of withdrawal can keep users on the hamster wheel of active opioid addiction, long after they want to get off.
And, as anyone in recovery knows, getting through withdrawal is only the beginning.
Those who manage to get through the dope sickness still have to contend with post-acute withdrawal symptoms, which can linger for anywhere from a few weeks for up to six months.
Suboxone can erase these hurdles.
2. Suboxone treatment on its own, though, won’t fix you
Suboxone alone is not likely to help you forge a new life.
It is like taking ibuprofen for a toothache. When it wears off, the problem is still there.
So, while Suboxone will allow you to function on a daily basis, it doesn’t address the psychological and behavioral issues that drove you to addiction.
Unresolved trauma from adverse childhood events, mental conditions, PTSD from combat, lack of coping skills and more factor into the development of addiction. Without addressing those factors, clients are likely to return to addiction after Suboxone treatment.
As one former user put it:
“’You can’t just say, ‘I can’t do this anymore. It’s ruining my life.’ You really have to dedicate yourself to this… because even a drug like Suboxone isn’t going to fix you. It’s you.’” (Kahill, 2016)
For this reason, Suboxone’s indications and usage state that it “should be used a part of complete treatment plan that includes counseling and psychosocial support.”
If you want to a full life and lasting recovery, look for a qualified Suboxone provider that offers the full range of evidence-based addiction treatment and support.
3. Suboxone treatment is not for everyone
There are some people who may not want to consider Suboxone treatment.
As with any medication, Suboxone comes with side effects. Because of this, any Suboxone treatment provider you choose should be concerned with your entire medical history, well-being and mental health.
For example, those with breathing problems such as chronic obstructive pulmonary disorder (COPD) will want to discuss these issues with a physician before beginning Suboxone treatment. Why? Because suboxone, just like other opioids, can suppress respiratory and central nervous system function.
Also, if you have a liver condition such as Hepatitis B or C, Suboxone treatment may not be for you. Buprenorphine, one of the active ingredients in Suboxone, can cause elevated liver enzyme levels, the destruction of liver cells, and death.
Those who have a head injury or intracranial lesions may want to use caution as well, as Suboxone can elevate the pressure of the fluid surrounding the brain and spine… a condition which can lead to severe headaches and/or vision loss.
Similarly, if you have problems or issues with your biliary tract, you will want to let your Suboxone treatment provider know. Opioids can raise intracholedochal pressure, otherwise known as the intensity of the flow of bile passing through the digestive system.
You could also experience adrenal insufficiency (a condition in which the body doesn’t make enough of certain hormones) and androgen deficiency (a condition in which the body is not making enough sex hormones). You can even be allergic to Suboxone.
For those who are pregnant, neonatal opioid withdrawal syndrome (NOWS) is a serious concern. There is also a risk of overdose if Suboxone is taken with other opioids or even other drugs such as cocaine.
Finally, there are certain medications that have been known to interact significantly with Suboxone, from alcohol and benzodiazepines to certain antiretrovirals, monoamine oxidase inhibitors and more. This also includes drugs such as selective serotonin reuptake inhibitors (SSRIs) that are used to treat depression.
RELATED: What is Suboxone and what is it used for?
Tell your Suboxone provider about all the medications you are taking. After beginning Suboxone treatment, be sure to tell any new provider, pharmacy or prescribing physician (or ER doctor if you have a trip there) that you are on Suboxone.
4. You can become dependent on Suboxone
Some would argue that “Suboxone is sober.” Not so, if it means experiencing extremely uncomfortable withdrawal symptoms and intense cravings when Suboxone is stopped. That sounds a lot more like opioid dependence.
But let’s hear from Suboxone users themselves:
“I’ve tried to get off Suboxone—it’s nearly impossible. I hate being like this and yes, I know I’m a slave to this chemical/opiate. After a solid week of hellish withdrawal, I caved in and got back on Subs. I had no idea what bad shape my body was in and how addicted I was until I quit. I was told I wouldn’t feel better for quite a time as the withdrawal can last forty days. Do you hear me? Forty full days. Makes you feel like you are literally dying without it.”
“Worst detox I ever had was coming off Suboxone, and I was a junkie for twelve years. It’s a joke to call this rehab, it’s switching one addiction for another.”
“To be honest, Suboxone ruined my life. My doctor had me prescribed for almost seven years. In those seven years, I relapsed at least once a year but most likely more. I knew that if I didn’t take a Sub for a few hours, I could sniff some dope. Suboxone was a crutch—a filler. One day (the last time), I said ‘Screw this, I don’t want to do Subs or dope anymore!’ So I detoxed myself from everything. Detoxing from Suboxone is the WORST!! I was in and out of the hospital six times in two weeks for IV fluids and comfort meds like Clonidine and muscle relaxers so I could sleep. For three and a half weeks, I didn’t move from my mother’s couch. Didn’t eat, barely slept… Long story short, Suboxone is the root of all evil. Eventually you WILL have to detox from them and I can tell you firsthand it won’t be easy.” (Narconon International, 2017)
It’s definitely easier to simply keep someone on Suboxone forever. It’s not the right thing to do, however. Freeing someone from one prison only to put them in another is not the answer.
If that is your provider’s philosophy about Suboxone treatment – keeping you on it forever – then it’s true that calling that treatment provider a “rehab” is a joke.
The bottom line is that the buprenorphine in Suboxone fits into the opioid category. It carries a risk of dependency.
This is why reputable Suboxone treatment programs will not keep clients on a long-term maintenance… and certainly not anywhere near seven years. After all, the goal is to recover from dependency on substances, not to instigate another lifelong medication that clients can become tolerant of and enslaved to.
Qualified Suboxone treatment programs are able to use Suboxone for the excellent tool that it is. They administer Suboxone to clients during withdrawal and maintain them on it during the treatment phase, allowing them get through acute and post-acute withdrawal periods comfortably as well as to participate in their recovery.
Afterward, clients are slowly and carefully weaned off Suboxone. (Keywords here are slowly and carefully). The dose can be always be adjusted back up temporarily to stop withdrawal symptoms should they rear their ugly heads… and then slowly tapered again.
As former long-term Suboxone users so eloquently illustrated above, Suboxone should not be abruptly stopped.
5. Your brain won’t heal on Suboxone
“’I’ve seen what long-term Suboxone does. People come in with endocrine problems – thyroid dysfunction, low testosterone… hair loss [and] tooth loss with Suboxone. There’s no way your brain chemistry can heal while on buprenorphine. You’re continuing to give someone a narcotic.”
– Dr. Steven Scanlan, psychiatrist and addiction specialist, formerly addicted to fentanyl (Matesa, 2011)
Long-term opioid use has consequences. For example, opioids have been known to cause fertility problems in both men and women.
Let’s focus on the brain for a minute, however.
One of the things that makes withdrawal from opiates so difficult is the changes to the brain that happen with opioid addiction.
For example, our brain becomes less responsive to normally pleasant activities like eating, exercising, playing a game or achieving a goal.
Neurotransmitters released in response to such activity bind to what are called mu receptors in the brain, activating them and releasing chemicals that feel pleasurable.
Opioids also bind to those receptors, flooding them with dopamine and causing an intense high – much more intense than what we would experience normally. The brain adapts by becoming less sensitive to dopamine as tolerance builds. Take the opioids away, and the brain needs more time to adapt to its new state.
Your brain also has an excellent survival mechanism built in: Things that make us feel good, we try to repeat. Your brain remembers the intense high and drives you to opioid use, again and again.
Also, whenever the level of opioids in your system happens to fall, your brain’s extended amygdala heightens negative feelings (cue the dope sickness). This also drives the repeated use of opioids.
And our CEO, the brain’s prefrontal cortex, responsible for impulse control and other executive functions, is short-circuited so many times it becomes underactive. This allows the addict to default straight to opioid use without consideration for the consequences.
These are but a few of the changes that affect behavior and keep addicts on that hamster wheel of addiction.
RELATED: How do drugs affect the brain?
So, when that hamster wheel finally stops, the brain has to recover.
This is a process which does not happen overnight. And it’s a process that won’t even start until Suboxone treatment is ceased.
Healing the brain takes two things: time and abstinence from opioids.
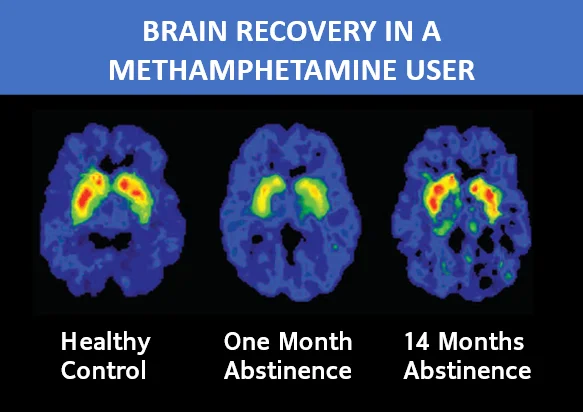
Take a look at these brain activity scans of a meth user who stopped using for 14 months. (Treatment and Recovery | National Institute on Drug Abuse, 2020):
As you can see, as soon as possible, it is good to taper off Suboxone treatment so that the clock on brain recovery can begin.
Get the Answers You Deserve Before Suboxone Treatment Begins
Suboxone is just like anything else: When used properly, it is a Godsend. When abused, it is the opposite.
Suboxone is a wonderful tool to keep withdrawal symptoms at bay so that you can get out of danger, get treatment, and start a new, clean life.
Just remember that Suboxone treatment is meant to be temporary. It’s a means to an end. It helps you get where you need to be – it is not the answer to all your problems.
With the help of properly timed Suboxone treatment, you can get the life you always wanted, with a minimum of discomfort and a maximum benefit from treatment.
The key is to get a Suboxone treatment provider you can trust. Make sure that you know the philosophy behind your Suboxone treatment provider’s operation, as well as how they administer it.
You have every right to ask questions… and get the answers you need, before you start Suboxone.
RELATED: Learn more about Foundations Wellness Center’s Suboxone treatment
Is it possible to overcome addiction?
What does it mean to have an addictive personality?
Sources
Institute on Drug Abuse. 2020. Treatment And Recovery | National Institute On Drug Abuse. [online] Available at: Drugabuse.gov [Accessed 23 June 2020].
Kahill, P., 2016. Why Are So Many Suboxone Patients Buying The Drug On The Street?. [online] Sideeffectspublicmedia.org. Available at: <https://www.sideeffectspublicmedia.org/post/why-are-so-many-suboxone-patients-buying-drug-street> [Accessed 23 June 2020].
Matesa, J., 2011. The Great Suboxone Debate | The Fix. [online] The Fix. Available at: <https://www.thefix.com/content/best-kept-secret-addiction-treatment?page=all> [Accessed 23 June 2020].
Rinker, B., 2019. What ‘Dope Sick’ Really Feels Like. [online] Kaiser Health News. Available at: <https://khn.org/news/what-dope-sick-really-feels-like/> [Accessed 23 June 2020].
Narconon International. 2017. Life On Suboxone: Not As Pretty As The Brochures Make You Think. [online] Available at: <https://www.narconon.org/blog/life-on-suboxone-not-as-pretty-as-the-brochures-make-you-think.html> [Accessed 23 June 2020].